Living well in surgical menopause
Our lifestyle can support us through surgical menopause, too - because you deserve to live well in this new chapter of your life.
Kate Dyson
Dr Emma Radway-Bright
Dr Sally Doust
Written By:
Medically Reviewed By:
Life after surgical menopause
Once the immediate recovery has passed, our next chapter is about rebuilding confidence, energy, and trust in our body again. Surgical menopause is not simply a medical event – it’s a profound physical and emotional transition. We’ve lost your natural source of oestrogen, progesterone and testosterone, but with the right treatment and care, we can protect our long-term health and feel well again.
Living well after ovary removal means working with our body. Hormones, nutrition, movement, and emotional support all play an important role. You deserve ongoing care, not just short-term recovery.
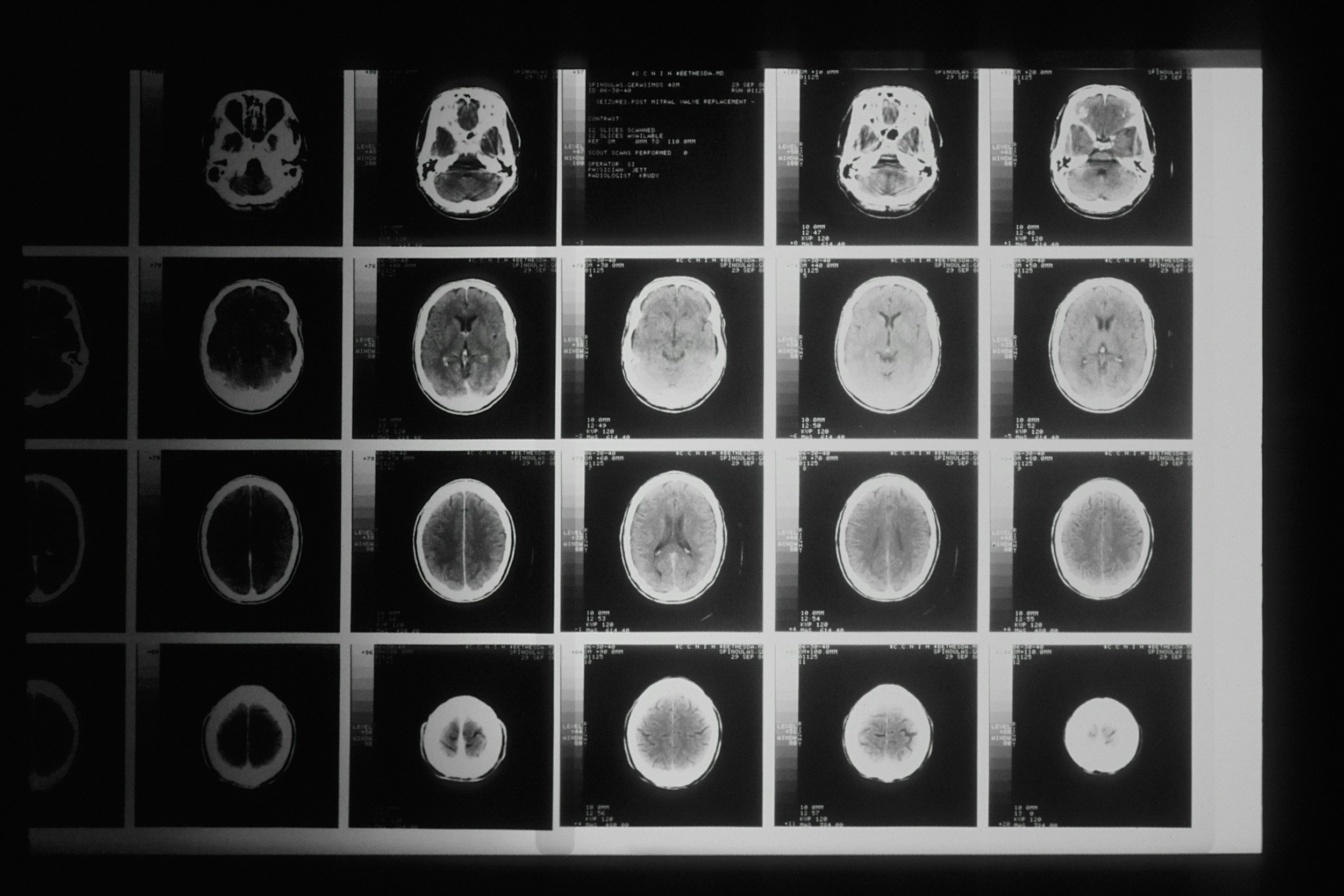
Protecting your heart, bones, and brain
The sudden loss of ovarian hormones affects the cardiovascular system, skeletal strength, and brain health. Without oestrogen, arteries can stiffen, cholesterol may rise, bone density declines, and cognitive function can be affected. These are not abstract risks — they are measurable, well-documented outcomes of untreated surgical menopause.
5 elements of good health in surgical menopause
Diet & nutrition
Supports healing, energy and bone health
Quality sleep & rest
Essential for recovery, hormones and emotional resilience
Strength & resistance exercise
Builds bone, muscle and long-term health (aim for 150 minutes weekly)
Self-care & mental wellness
Supports emotional wellbeing through hormonal change
Support & appropriate treatment
Individualised care to protect long-term health, including HRT if appropriate for you.
Elements of good health in surgical menopause
Diet & Nutrition
Supports healing, energy levels & bone health before and after surgery
Support & Appropriate Treatment
Medical treatment, including HRT where appropriate, should be individualised and reviewed regularly
Self-care & Mental Wellness
Supports emotional resilience during major hormonal and life change
Strength & Resistance Exercise
Helps protect bones, build strength and support long-term health (around 150 minutes a week)
Quality Sleep & Rest
Plays a vital role in recovery, hormone balance and emotional wellbeing
Advice to help you live well
Hormones
If you are able to take hormone replacement therapy, it plays a central role in protecting long-term health after ovary removal. Oestrogen helps keep blood vessels flexible, supports bone density, and protects brain cells from inflammation. Research consistently shows that women who start HRT soon after surgical menopause have better cardiovascular, cognitive and skeletal outcomes over time.
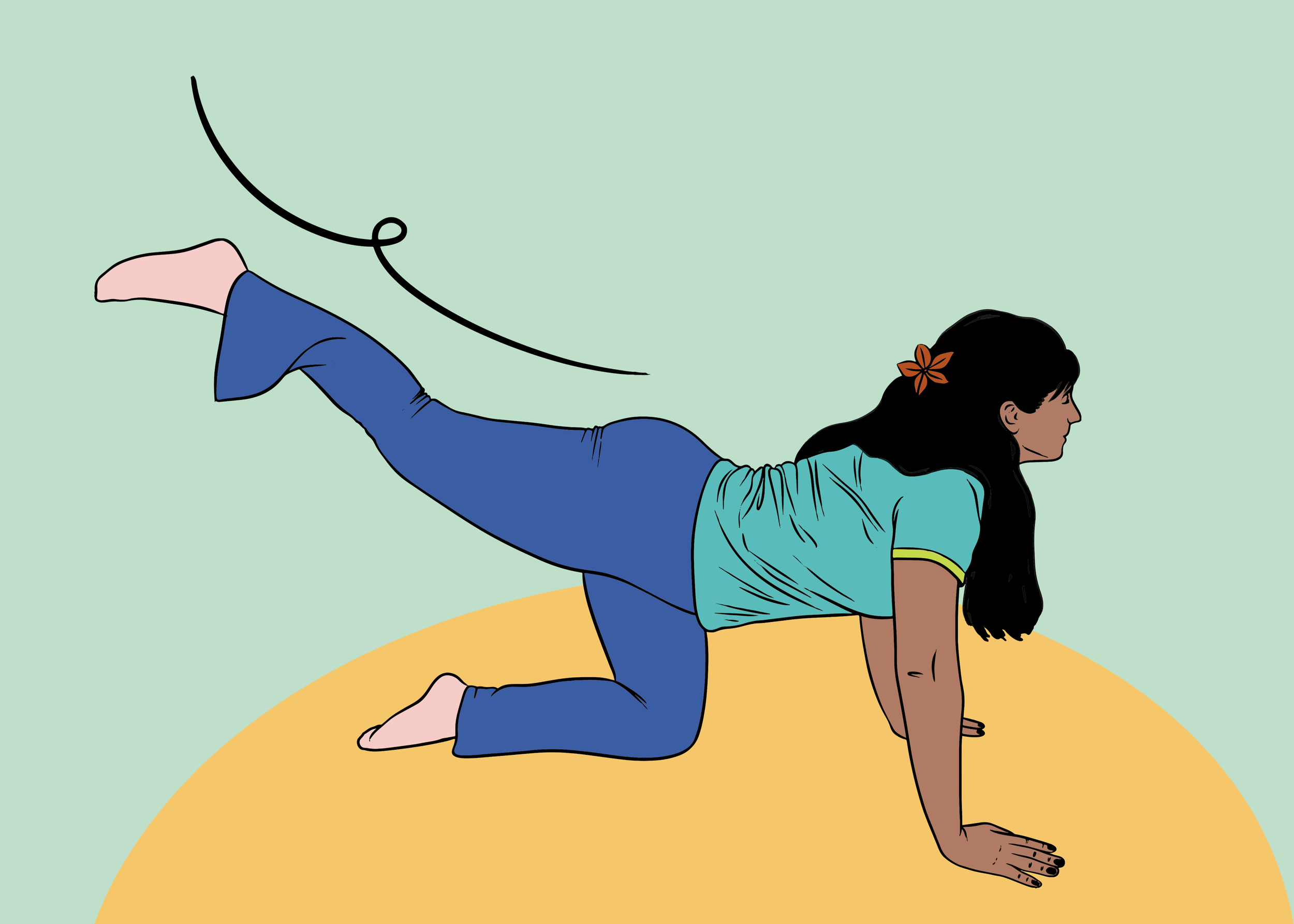
Movement
Exercise really is medicine. Movement is one of the most powerful tools for protecting health in surgical menopause. Weight-bearing activities such as walking, dancing, yoga and resistance training help maintain bone strength and support heart health. Even small amounts count. Regular, consistent movement matters far more than intensity, and strength training in particular has been shown to support bone density, muscle mass and metabolic health during menopause.
Nutrition
Good nutrition provides the building blocks your body needs to adapt after surgery. Calcium and vitamin D are essential for maintaining bone strength, while adequate protein supports muscle maintenance and tissue repair. Omega-3 fats help regulate inflammation and support brain health. A varied diet rich in fruit, vegetables and whole grains supports hormone metabolism, cardiovascular health and long-term resilience.
Sleep
Sleep is a cornerstone of recovery and long-term health, not a luxury. Quality sleep supports hormone regulation, brain function, immune health and emotional resilience. Ongoing sleep disruption increases inflammation, affects blood sugar regulation and can worsen mood, memory and fatigue, making sleep care an essential part of protecting your health after surgical menopause.
Lifestyle
Everyday choices can meaningfully influence long-term outcomes. Stopping smoking helps slow bone loss and protects blood vessels, while limiting alcohol supports bone, brain and sleep health. Regular health checks allow early monitoring of blood pressure, cholesterol, blood sugar and bone density, helping you address changes early rather than react later.
Together, these small but steady actions help your body remain strong, adaptable and well-supported, even without natural ovarian hormones.
Your brain in surgical menopause
Our hormones influence the brain more than most people realise. Oestrogen supports blood flow and protects neurons; progesterone and testosterone affect mood, memory, and motivation. When they suddenly disappear, it’s normal to feel “foggy”, tearful, or less like yourself.
For those of us who are able to take HRT, we will find that cognitive symptoms often ease over time as we reach optimum hormone health. But it’s not the only thing we need to do to support our long term brain health, and for those unable to take HRT in surgical menopause, the following are proven to support cognitive health and our mental wellbeing.
Prioritising sleep, even if that means daytime rest.
Managing stress through breathing exercises, journalling, or gentle mindfulness.
Staying socially connected – isolation increases cognitive decline risk.
Keeping your mind active by reading, playing music, doing puzzles, or learning something new. These activities all help maintain neural health.
If your brain fog or memory issues persist even after starting HRT, ask your clinician about checking your thyroid, B12, and iron levels. Sometimes it’s a combination of factors that mean we continue to feel this particular symptom of surgical menopause.
Pelvic floor and urinary health
Your pelvic floor is a powerful network of muscles that supports your bladder, bowel and vagina. After ovary removal, the sudden loss of oestrogen can cause these muscles and tissues to become thinner and less elastic, which can make leaks, urgency, or prolapse symptoms more noticeable. The good news is that these changes are common, reversible, and respond well to the right support.
Start with awareness.
Try to consciously relax and engage your pelvic floor each day. Most women are told to “squeeze,” but the release is just as important. Think of it as a lift that goes both up and down – you want it to move freely, not stay tense.
Oestrogen supports the structure.
Local vaginal oestrogen keeps the pelvic tissues plump, flexible and better able to support the bladder and urethra. It’s safe to use long term, even if you can’t use systemic HRT. If you can, it can be combined with HRT.
Daily exercises do work.
Short, regular pelvic floor sessions are more effective than occasional long ones. Focus on a few slow, strong lifts and a few quick pulses, breathing normally throughout. Apps or guided audio programmes can help you build consistency.
Stay hydrated – but smartly.
It’s tempting to drink less when you’re leaking, but dehydration irritates the bladder and makes urgency worse. Aim for light-yellow urine and limit caffeine, fizzy drinks, and alcohol if you’re struggling with frequency.
Women’s health physiotherapy can make a huge difference.
A specialist pelvic health physio can assess your strength, teach correct technique, and check for signs of prolapse. Many offer virtual consultations if travel or waiting lists are difficult.
Pee properly to empty your bladder.
Rushing, hovering, or pushing can leave urine behind and irritate the bladder. Sit fully, relax your jaw and pelvic floor, take your time, and try a gentle lean forward or double voiding to help the bladder empty more completely.
Supporting you to live well at every stage
The latest research, experiences and advice to support you through surgical menopause.